COMEDOGENIC AND DERMATITIS
Comedogenic
tending to cause blackheads by blocking the pores of the skin.
"Comedo" is Latin for blackhead - dirt or fatty matter in a skin duct. "Genic" means "producing" or "favoring"- as in photogenic.
Comedogenic therefore literally means "blackhead causing", and is conventionally accepted to be acne-causing, since clogged pores are an important cause of acne.
The average adult has around 5 million pores on his skin (one for each hair, which is all over the body, even if invisible). Ingredients that have the tendency to accumulate in the pores and jam them up are comedogenic. Ingredients that do not have this tendency are non-comedogenic. These are the two extremes, and there are lots of ingredients in between.
The skin is a very active organ within, although it looks calm on the outside. When pores clog, the natural excretion of sebum and dead cells from the skin reduces. This leads to, you guessed it - comedos! This build-up is a great place for bacteria to establish themselves, and when they do that, the skin responds with redness and swelling, which is what we see as acne or pimples
Acne is a chronic, inflammatory skin condition that causes spots and pimples, especially on the face, shoulders, back, neck, chest, and upper arms.
Whiteheads, blackheads, pimples, cysts, and nodules are all types of acne.
It is the most common skin condition in the United States, affecting up to 50 million Americans yearly. It commonly occurs during puberty, when the sebaceous glands activate, but it can occur at any age. It is not dangerous, but it can leave skin scars.
The glands produce oil and are stimulated by male hormones produced by the adrenal glands in both males and females.
At least 85 percent of people in the U.S. experience acne between the ages of 12 and 24 years. Acne pimples vary in size, color, and level of pain.
The following types are possible:
• Whiteheads: These remain under the skin and are small
• Blackheads: Clearly visible, they are black and appear on the surface of the skin
• Papules: Small, usually pink bumps, these are visible on the surface of the skin
• Pustules: Clearly visible on the surface of the skin. They are red at their base and have pus at the top
• Nodules: Clearly visible on the surface of the skin. They are large, solid, painful pimples that are embedded deep in the skin
• Cysts: Clearly visible on the surface of the skin. They are painful and filled with pus. Cysts can cause scars.
Causes
Human skin has pores that connect to oil glands under the skin. Follicles connect the glands to the pores. Follicles are small sacs that produce and secrete liquid.
The glands produce an oily liquid called sebum. Sebum carries dead skin cells through the follicles to the surface of the skin. A small hair grows through the follicle out of the skin.
Pimples grow when these follicles get blocked, and oil builds up under the skin.
Skin cells, sebum, and hair can clump together into a plug. This plug gets infected with bacteria, and swelling results. A pimple starts to develop when the plug begins to break down.
Propionibacterium acnes (P. acnes) is the name of the bacteria that live on the skin and contributes to the infection of pimples.
Research suggests Trusted that the severity and frequency of acne depend on the strain of bacteria. Not all acne bacteria trigger pimples. One strain helps to keep the skin pimple-free.
Hormonal factors
A range of factors triggers acne, but the main cause is thought to be a rise in androgen levels.
Androgen is a type of hormone, the levels of which rise when adolescence begins. In women, it gets converted into estrogen.
Rising androgen levels cause the oil glands under the skin to grow. The enlarged gland produces more sebum. Excessive sebum can break down cellular walls in the pores, causing bacteria to grow.
Other possible triggers
Some studies suggest that genetic factors may increase the risk.
Other causes include:
• some medications that contain androgen and lithium
• greasy cosmetics
• hormonal changes
• emotional stress
• menstruation
Treatment
Treatment depends on how severe and persistent the acne is.
Mild acne
Mild acne can be treated with over-the-counter (OTC) medications, such as gels, soaps, pads, creams, and lotions, that are applied to the skin.
Creams and lotions are best for sensitive skin. Alcohol-based gels dry the skin and are better for oily skin.
OTC acne remedies may contain the following active ingredients:
• Resorcinol: helps break down blackheads and whiteheads
• Benzoyl peroxide: kills bacteria, accelerates the replacement of skin, and slows the production of sebum
• Salicylic acid: assists the breakdown of blackheads and whiteheads and helps reduce inflammation and swelling
• Sulfur: exactly how this works is unknown
• Retin-A: helps unblock pores through cell turnover
• Azelaic acid: strengthens cells that line the follicles, stops sebum eruptions, and reduces bacterial growth. There is cream for acne, but other forms are used for rosacea.
It is advisable to start with the lowest strengths, as some preparations can cause skin irritation, redness, or burning on first use.
These side effects normally subside after continued use. If not, see a doctor.
Treating moderate to severe acne
A skin specialist, or dermatologist, can treat more severe cases.
They may prescribe a gel or cream similar to OTC medications but stronger, or an oral or topical antibiotic.
Corticosteroid injection
If an acne cyst becomes severely inflamed, it may rupture. This can lead to scarring.
A specialist may treat an inflamed cyst by injecting a diluted corticosteroid.
This can help prevent scarring, reduce inflammation, and speed up healing. The cyst will break down within a few days.
Oral antibiotics
Oral antibiotics may be prescribed for up to 6 months for patients with moderate to severe acne.
These aim to lower the population of P. Acnes. The dosage will start high and reduce as the acne clears.
P. acnes can become resistant to the antibiotic in time, and another antibiotic is needed. Acne is more likely to become resistant to topical rather than oral antibiotics.
Antibiotics can combat the growth of bacteria and reduce inflammation.
Erythromycin and tetracycline are commonly prescribed for acne.
Oral contraceptives
Oral contraceptives can help control acne in women by suppressing the overactive gland. They are commonly used as long-term acne treatments.
These may not be suitable for women who:
• have a blood-clotting disorder
• smoke
• have a history of migraines
• are over 35 years old
It is important to check with a gynecologist first.
Topical antimicrobials
Topical antimicrobials also aim to reduce P. acnes in patients with moderate to severe acne. Examples are clindamycin and sodium sulfacetamide.
The dermatologist may prescribe a topical retinoid.
Topical retinoids are a derivative of vitamin A. They unclog the pores and prevent whiteheads and blackheads from developing.
Examples of topical retinoids prescribed in the U.S. are adapalene, tazarotene, and tretinoin.
Isotretinoin
This is a strong, oral retinoid, used for the treatment of severe cystic acne and severe acne that has not responded to other medications and treatments.
It is a strictly controlled medication with potentially serious side effects. The patient must sign a consent form to say that they understand the risks.
Adverse effects include dry skin, dry lips, nosebleeds, fetal abnormalities if used during pregnancy, and mood swings.
Patients who take isotretinoin must avoid vitamin A supplements, as these could lead to vitamin A toxicity.
Dermatitis
Overview
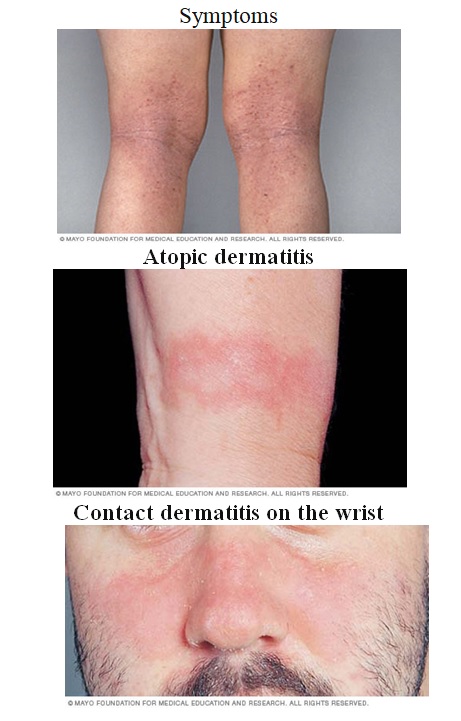
Dermatitis is a general term that describes a skin irritation. Dermatitis is a common condition that has many causes and occurs in many forms. It usually involves itchy, dry skin or a rash on swollen, reddened skin. Or it may cause the skin to blister, ooze, crust or flake off. Examples of this condition are atopic dermatitis (eczema), dandruff and contact dermatitis.
Dermatitis isn't contagious, but it can make you feel uncomfortable and self-conscious. Moisturizing regularly helps control the symptoms. Treatment may also include medicated ointments, creams and shampoos.
Types
1. Atopic dermatitis (eczema)
2. Contact dermatitis
3. Cradle cap
4. Diaper rash
5. Seborrheic dermatitis
Seborrheic dermatitis on the face
Each type of dermatitis may look a little different and tends to occur on different parts of your body. Signs and symptoms of different types of dermatitis include:
• Atopic dermatitis (eczema). Usually beginning in infancy, this red, itchy rash usually occurs where the skin flexes — inside the elbows, behind the knees and in front of the neck. The rash may leak fluid when scratched and crust over. People with atopic dermatitis may experience improvement and then seasonal flare-ups.
• Contact dermatitis. This red, itchy stinging rash occurs where your skin has come into contact with substances that irritate the skin or cause an allergic reaction. You may develop blisters.
• Seborrheic dermatitis. This condition causes scaly patches, red skin and stubborn dandruff. It usually affects oily areas of the body, such as the face, upper chest and back. Seborrheic dermatitis can be a long-term condition with periods of improvement and then seasonal flare-ups. In infants, this condition is called cradle cap.
• Follicular eczema. With this type, the affected skin thickens and develops bumps in hair follicles. This condition is common in African Americans and in people with dark-brown skin.
Causes of the most common types of dermatitis include:
• Atopic dermatitis (eczema). This type is likely related to dry skin, a gene variation, an immune system dysfunction, a skin infection, exposure to food, airborne, or contact allergens, or a combination of these.
• Contact dermatitis. This type results from contact with something that irritates your skin or causes an allergic reaction. Irritants or allergens include poison ivy, perfumes, jewelry containing nickel, cleaning products, and the preservatives in many creams and lotions.
• Seborrheic dermatitis. This type is caused by a yeast (fungus) that is in the oil secretion on the skin. Risk factors
Common risk factors for dermatitis include:
• Age. Dermatitis can occur at any age, but atopic dermatitis (eczema) usually begins in infancy.
• Allergies and asthma. People who have a personal or family history of eczema, allergies, hay fever or asthma are more likely to develop atopic dermatitis.
• Occupation. Jobs that put you in contact with certain metals, solvents or cleaning supplies increase your risk of contact dermatitis. Being a health care worker is linked to hand eczema.
• Health conditions. Health conditions that put you at increased risk of seborrheic dermatitis include congestive heart failure, Parkinson's disease and HIV/AIDS.
Complications
Scratching the itchy rash associated with dermatitis can cause open sores, which may become infected. These skin infections can spread and may very rarely become life-threatening.
Prevention
Wear protective clothing if you are doing a task that involves irritants or caustic chemicals.
Avoid dry skin by adopting these habits when bathing:
• Take shorter baths and showers. Limit your baths and showers to 5 to 10 minutes. Use warm, rather than hot, water. Bath oil also may be helpful.
• Use a gentle, nonsoap cleanser. Choose unscented nonsoap cleansers. Some soaps can dry your skin. • Dry yourself gently. After bathing, gently pat your skin dry with a soft towel.
• Moisturize your skin. While your skin is still damp, seal in moisture with an oil, cream or lotion. Try different products to find one that works for you. Ideally, the best one for you will be safe, effective, affordable and unscented. Two small studies showed that applying a protective moisturizer to the skin of infants at high risk of atopic dermatitis reduced the incidence of the condition by up to 50 percent.